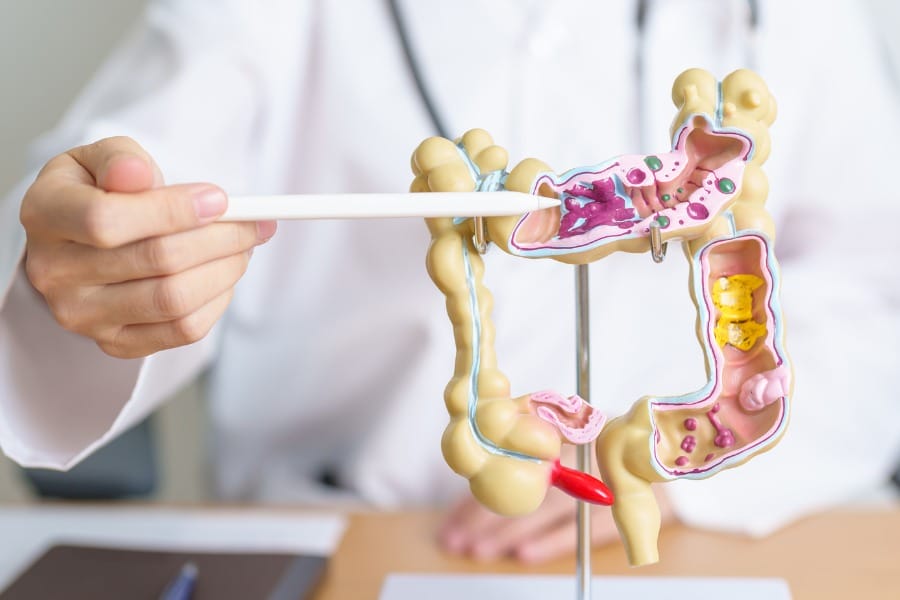
Diverticular disease is a common illness that forms in the large intestine as individuals age.
During digestion, food travels along the large intestine.
Over time, the walls of the large intestine can lose strength. Some spots will weaken so much so that they will start to bulge outward, forming small pockets calls diverticula. The pockets usually do not cause any problems.
Diverticula are actually quite common, especially in individuals who are over the age of forty.
It is estimated that about 65% of adults will develop diverticular disease by the age of 80. About 10 to 30% of people with diverticular disease will suffer complications such as diverticulitis and/or diverticular bleeding.
Diverticulitis only occurs when these pockets become infected or inflamed. This can lead to extreme abdominal pain and may require surgery in some cases. However, mild diverticulitis can be treated with rest and lifestyle adjustments.
Understanding Diverticulitis is important because it is a condition that can cause discomfort and lead to serious complications if left untreated.
Symptoms of diverticulitis can range from mild to severe, and they can mimic other digestive disorders. Diagnosis typically involves a physical exam, medical history, and imaging tests.
Treatment options may include antibiotics, pain management, and dietary changes. In some cases, surgery may be necessary to remove the affected portion of the colon.
Key Takeaways
- Diverticulitis is a condition that affects the colon and occurs when the diverticula becomes inflamed or infected.
- Symptoms of diverticulitis can range from mild to severe and can mimic other digestive disorders.
- Treatment options for diverticulitis may include antibiotics, pain management, dietary changes, and surgery if necessary.
Causes of Diverticulitis
IN THIS ARTICLE
The exact cause of diverticulitis is unknown. However, it is believed that a low-fiber diet and a sedentary lifestyle may contribute to its development.
When there is not enough fiber in the diet, the stool becomes harder and more difficult to pass, which can lead to increased pressure on the colon
Diverticula like to develop when a spot in your colon gives way under pressure. This causes olive-sized pouches to break through the colon wall. When the diverticula breaks, inflammation or infection can occur.
Prevalence and Risk Factors of Diverticulitis
Diverticulitis is a common condition, especially in older adults.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), about half of all Americans over the age of 60 have diverticulosis, which is the condition of having diverticula. However, only a small percentage of people with diverticulosis develop diverticulitis.
Risk factors for diverticulitis include age, obesity, smoking, lack of exercise, and a diet low in fiber.
People with a family history of diverticulitis are also at increased risk. Women may be more likely to develop diverticulitis than men.
There are a variety of factors that contribute to the risk of developing diverticulitis.
- This illness becomes increasingly common as people age. It is diagnosed more often in people over the age of forty.
- Obesity is associated with a number of digestive diseases, and it can increase the chance of developing diverticulitis too. Similarly, a low-fiber diet increases the risk of diverticulitis.
- Individuals who smoke cigarettes are at a higher risk for developing diverticular disease and diverticulitis than those who do not smoke.
- Lack of exercise. Little or no exercise has been found to increase the risk of diverticulitis.
- Abundance of red meat. Doctors are not sure why, or what constitutes too much, but eating a lot of red meat can trigger diverticulitis. Try consuming leaner meats, like chicken or fish.
- Certain medications.A few drugs, such as steroids, opioids, and medications related to ibuprofen and naproxen sodium, are known to put an individual at a greater risk of developing diverticulitis.
Symptoms of Diverticulitis
Symptoms may not always be obvious in cases of diverticulitis.
The most common symptom people have is sharp pain in the lower left abdominal region. Other symptoms include nausea, chills, cramping, changes in bowel movements, and fever.
Diverticulitis can cause various symptoms, including:
- Abdominal pain, which is usually felt on the lower left side, but may also occur on the right side in people of Asian descent
- Nausea and vomiting
- Constipation or diarrhea
- Bloating and gas
- Fever and chills
The symptoms of diverticulitis may vary depending on the severity of the condition. Some people may only experience mild symptoms, while others may have severe symptoms that require hospitalization.
Prevention
The best way to prevent diverticulitis is by maintaining a healthy lifestyle. The following methods will help you reduce the risk of getting diverticulitis.
- Exercise regularly. Exercise will reduce the pressure inside the colon and will aid in normal bowel function. Exercise does not need to be intense. Simply walking every day is great, so long as it is maintained regularly.
- Eat more fiber. A diet that is filled with fiber will decrease the risk of diverticulitis. Foods high in fiber such as whole grains and vegetables will soften waste material and allow it to pass faster through the colon.
- Drink plenty of fluids. When you increase your fiber intake, you will need to increase your intake of fluids too. Fluids act as natural lubricants within the body’s digestive tract. Stay hydrated by drinking the recommended 8 glasses of water a day.
Diagnosis and Treatment
If a person is experiencing symptoms of diverticulitis, a doctor will perform a physical examination to check for tenderness in the abdomen. Women may also have a pelvic exam to rule out other conditions.
In addition to a physical exam, a doctor may order diagnostic tests to confirm a diagnosis of diverticulitis. These tests may include:
- Blood tests to check for signs of infection
- Stool tests to check for the presence of blood or infection
- Imaging tests, such as a CT scan or ultrasound, to visualize the colon and identify any inflammation or infection
It is important to seek medical attention if you are experiencing symptoms of diverticulitis, as prompt diagnosis and treatment can help prevent complications.
Diverticulitis can be difficult to diagnose.
Typically, it will go undiagnosed until the symptoms occur.
A person with diverticulitis may only know they have the disease once they experience extreme stomach pain and go to the hospital. However, it is common for physicians to find diverticulitis when looking for the cause of other symptoms or during a routine colonoscopy.
There are some distinct lab tests that can be beneficial for determining whether or not an individual has diverticulitis. These tests include:
Colonoscopy. This test is usually performed to check out symptoms relating to bleeding or abdominal pain. It is a required routine screening for people over the age of 50. A colonoscopy can lead to the diagnosis of asymptomatic diverticular disease. From there, the patient may be able to make lifestyle adjustments to prevent diverticulitis.
Computerized Tomography Scan. This scan consists of a series of x-rays that offer a view of the abdomen and other areas of the body. This scan is usually non-invasive and painless. In some instances, a dye is used to strengthen the visibility of some structures. The dye helps medical professionals visualize organs in the body and look for anything out of the ordinary, like diverticula.
Surgical Interventions
Surgical interventions may be necessary if the patient experiences complications such as abscesses, fistulas, or bowel obstructions. In some cases, surgery may be recommended to remove the affected part of the colon.
This is usually done laparoscopically, which involves making small incisions in the abdomen and using a camera and specialized instruments to remove the affected tissue.
Complications and Management of Diverticulitis

Potential Complications
While most cases of diverticulitis are mild and can be treated with antibiotics and lifestyle changes, some individuals may experience complications. According to Mayo Clinic, about 25% of people with acute diverticulitis develop complications. These complications may include:
- An abscess, which occurs when pus collects in the pouch.
- A fistula, which is an abnormal connection between two organs or between an organ and the skin.
- A bowel obstruction, which occurs when the intestine is partially or completely blocked.
- Peritonitis, which is inflammation of the lining of the abdominal cavity.
Severe or persistent diverticulitis can also lead to complications such as gastrointestinal bleeding and intestinal obstruction. Bleeding from diverticula can be severe and lead to anemia, while severe swelling might cause the colon to temporarily narrow.
Long-Term Management
After an episode of diverticulitis, individuals may need to make long-term lifestyle changes to prevent future episodes and manage the condition. These lifestyle changes may include:
- Eating a high-fiber diet to help soften stools and prevent constipation.
- Drinking plenty of fluids to help prevent constipation.
- Exercising regularly to help promote bowel regularity.
- Avoiding foods that may trigger symptoms, such as nuts, seeds, and popcorn.
- Taking probiotics to help restore healthy gut bacteria.
In some cases, surgery may be necessary to remove the affected part of the colon. This may be recommended for individuals who experience recurrent episodes of diverticulitis or who develop complications such as a bowel obstruction. The decision to undergo surgery should be made in consultation with a healthcare provider.
Prevention Strategies
While diverticulitis is a common condition, there are several strategies that individuals can employ to lower their risk of developing it. Here are some of the most effective prevention strategies:
1. Exercise Regularly
Regular exercise is a crucial component of maintaining a healthy colon. Exercise helps promote normal bowel function and reduces pressure inside the colon, which can help prevent the formation of diverticula. It is recommended that individuals engage in at least 30 minutes of moderate exercise on most days of the week.
2. Eat More Fiber
A high-fiber diet is essential for preventing diverticulitis. Fiber-rich foods, such as fresh fruits and vegetables, whole grains, and legumes, help soften stool and promote regular bowel movements. This reduces the pressure inside the colon and helps prevent the formation of diverticula. It is recommended that individuals consume at least 25-30 grams of fiber per day.
3. Drink Plenty of Fluids
Drinking plenty of fluids is important for maintaining regular bowel function and preventing constipation. It is recommended that individuals consume at least eight 8-ounce glasses of water per day. If an individual increases their fiber intake, they should also increase their fluid intake to prevent constipation.
4. Avoid Refined Foods
Refined foods, such as white flour, white rice, and other processed foods, should be avoided. These foods are low in fiber and can contribute to constipation, which can increase the risk of diverticulitis.
5. Avoid Red Meat
Red meat should be avoided or consumed in moderation. Studies have shown that a diet high in red meat may increase the risk of diverticulitis. Instead, individuals should opt for lean protein sources, such as fish, poultry, and plant-based proteins.
By following these prevention strategies, individuals can reduce their risk of developing diverticulitis and maintain a healthy colon.
Get Help Today
During urgent or serious cases, surgery can be performed. Every year, about 200,000 people are hospitalized for diverticulitis. Individuals who are diagnosed with diverticular disease should speak with a medical professional about which treatment plan is best for them in order to reduce the risk of diverticulitis. People should always speak to their doctor or a specialized gastroenterologist with any specific questions.
For people who been hospitalized for diverticulitis, a private duty nurse can help with recovery care to get you back home quickly and safely. Nurses are available for short, hourly visits or overnight care. If you would like to learn more about how a skilled nurse can help with your care, call 650-462-1001 to speak with a Client Care Coordinator. You can also view our Post-Hospital Discharge Planning Guide for free.
Frequently Asked Questions about Diverticulitis
What are the typical symptoms of diverticulitis?
Diverticulitis is characterized by pain in the lower left side of the abdomen, which can be constant and persist for several days. Nausea, vomiting, fever, and chills may also occur. In some cases, the right side of the abdomen may be more painful, especially in people of Asian descent.
How can diverticulitis be effectively treated?
The treatment of diverticulitis depends on the severity of the condition. Mild cases can be treated with rest, a liquid diet, and antibiotics. More severe cases may require hospitalization, intravenous antibiotics, and surgery.
When should someone with diverticulitis seek hospital care?
If the symptoms of diverticulitis are severe or if there is a high fever, hospitalization may be necessary. Additionally, if there is rectal bleeding, persistent vomiting, or signs of dehydration, medical attention should be sought immediately.
What dietary changes are recommended for those with diverticulitis?
A high-fiber diet is recommended for those with diverticulitis. This can help prevent the formation of diverticula and reduce the risk of diverticulitis. Foods such as fruits, vegetables, whole grains, and beans are good sources of fiber.
How can one distinguish between diverticulosis and diverticulitis?
Diverticulosis refers to the presence of diverticula, or small pouches, in the colon. This condition is usually asymptomatic. Diverticulitis, on the other hand, is a complication of diverticulosis that occurs when one of the pouches becomes inflamed or infected.
What foods are known to exacerbate diverticulitis symptoms?
Foods that are low in fiber, such as processed foods, red meat, and dairy products, can exacerbate diverticulitis symptoms. Additionally, foods that are difficult to digest, such as nuts, seeds, and popcorn, can irritate the colon and increase the risk of diverticulitis.
Resources
The Gastrointestinal Society offers a variety of resources for individuals with diverticulitis.
Helpful resources can be found on the American College of Gastroenterology webpage.
The American Gastroenterological Association has plenty of information to help cope with the illness and prevent recurrences.
American Society for Gastrointestinal Endoscopy offers guidance on fiber-rich foods to include in your diet.
Disclaimer: The information provided in this article is not intended to diagnose health problems or take the place of professional medical advice or care you receive from a health care provider. A diagnosis for diverticulitis must be confirmed with a licensed medical professional. Always consult your healthcare provider about symptoms, health problems, medications, and treatments.





