Lyme disease is an illness caused by four main species of bacteria, which include Borrelia burgdorferi, Borrelia mayonii, Borrelia afzelii, and Borrelia garinii bacteria. Borrelia burgdorferi and Borrelia mayonii are the leading causes of Lyme disease in the United States, while Borrelia afzelii and Borrelia garinii are the main causes of Lyme disease in Europe and Asia.
Lyme disease is a tick-borne illness that is transmitted to humans via the bite of an infected blacklegged tick, also known as a deer tick. Lyme disease cannot be transferred from person to person. This post will cover the following topics on Lyme disease:
Causes of Lyme Disease
Risk Factors
Symptoms of Lyme Disease
Lyme Disease Prevention
Diagnosis and Treatment of Lyme Disease
Resources
Causes of Lyme Disease
IN THIS ARTICLE
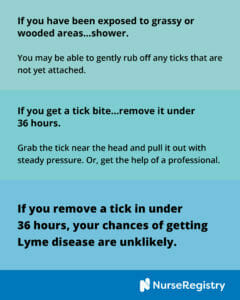
A person can contract Lyme disease when they are bitten by a tick. This is more likely to happen in grassy or heavily wooded areas where infected ticks thrive. The risk of disease is also more likely the longer the tick is attached. In most cases, a tick must be attached for 36 to 48 hours to transmit the disease. If the tick is removed in less than 36 to 48 hours, the risk of disease is unlikely.
Risk Factors
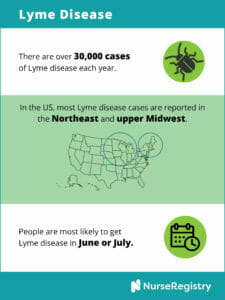
Common risk factors for Lyme disease include:
- Grassy or woody areas. Deer ticks thrive in heavily wooded or grassy areas. Young ticks prey on mice and other rodents, which often carry Lyme disease bacteria. Adult deer ticks prey on white-tailed deer. Children and adults who spend a lot of time in these areas are at an increased risk for developing Lyme disease. In the United States, Lyme disease is more prevalent in the Northeast and Midwest regions.
- Exposed skin. Ticks attach more easily to bare skin. If you plan on going out in grassy or woody areas, cover up. Wear long pants and long-sleeved shirts. Don’t allow pets to play in tall weeds and grasses.
- Not removing ticks quickly or properly. If a tick is removed properly in under 36 to 48 hours, the risk of Lyme disease is unlikely. Make sure to check for ticks after spending time in grassy or wooded areas. If you notice symptoms of Lyme disease, consult a doctor immediately.
Symptoms of Lyme Disease
Once a person is infected, symptoms usually appear in stages. Although they may vary from person to person, symptoms usually appear in the following order.
Immediate Symptoms
A small red bump will appear at the site of the tick bite or tick removal. This usually goes away within a few days. This does not indicate Lyme disease; all tick bites will result in a small red bump.
Early Stage Symptoms
Within 30 days of receiving a bite from an infected tick, you may notice the following symptoms:
- Rash (erythema migrans). This particular rash is one of the hallmarks of Lyme’s disease. It forms between 3 to 30 days after an infected tick bite. It is distinctly known for its bull’s eye pattern. The red area of the rash may expand outwards in a circle, and the center of the rash may be clear. Typically, the rash is not itchy or painful. It may continue to spread slowly, getting as large as 12 inches across. Some develop this rash in multiple places.
- Flu-like symptoms. The rash may be accompanied by flu-like symptoms such as fever, chills, fatigue, body aches, and a headache.
Late Stage Symptoms
If Lyme disease is left untreated, worsening symptoms may develop. These include:
- Rash (erythema migrans). The rash will continue to spread to other parts of the body.
- Joint pain. An infected person may experience extreme joint pain and swelling. Often, joint pain is experienced in the knees, but it can shift from one joint to another.
- Muscle pain and weakness. Muscle pain may not have a trigger point location. Some people may not be able to walk or stand due to muscle weakness. People may also experience stiffness in the neck or upper back.
- Sleep disturbances. People may sleep too much or not enough. Some may experience night terrors or anxiety.
- Gastrointestinal pain. Nausea and other digestive issues may occur.
- Changes in mood. Adults and children may experience mood swings and/or personality changes. Lyme disease is a known trigger for pediatric acute-onset neuropsychiatric syndrome (PANS). With this, children seemingly change overnight. They will have bursts of aggression or display OCD-type behaviors.
- Neurological problems. Serious neurological problems can develop weeks, months, or even years after being infected, which is why it’s so important to get diagnosed and treated quickly. Symptoms can include meningitis (inflammation of the membranes surrounding the brain), Bell’s palsy (temporary paralysis on one side of the face), impaired muscle movement, and numbness or weakness in the limbs.
If the infection is caused by the bacterium Borrelia mayonii, symptoms may also include:
- Nausea and vomiting
- Diffuse rashes (a rash that is spread out over multiple areas, rather than a single bull’s eye rash)
Some people may also develop these less common symptoms:
- Inflammation of the eye
- Hepatitis
- Severe fatigue
- Heart problems, including irregular heartbeat (these rarely last longer than a few weeks)
Symptoms When Left Untreated
If left untreated, Lyme disease can cause serious problems over time. These include:
- Lyme arthritis, or chronic joint inflammation (this often affects the knees)
- Neurological symptoms, such as facial palsy and neuropathy
- Cognitive defects, such as impaired memory
- Heart problems, such as irregular heart beat
When young, blacklegged ticks are no bigger than a poppy seed. This makes them difficult to spot.
If you do find an attached tick, contact a doctor immediately. Treatment is more effective when begun early.
If you notice symptoms of Lyme’s disease and they disappear, it is still important to contact your doctor. The absence of symptoms does not mean the disease is gone, and it can spread to other parts of the body. Over years, Lyme’s disease can cause arthritis and problems with the nervous system.
Lyme Disease Prevention
The best way to prevent Lyme disease is to avoid areas where deer ticks live. If that is not possible, the following methods can help you reduce the risk of contracting Lyme disease.
- Cover bare skin. Ticks attach to bare skin more easily. Make sure to cover up by wearing long pants and long-sleeved shirts. Consider tucking your pants into long socks, and wearing a hat and gloves.
- Avoid walking through tall grass. If you are in a grassy or wooded areas, try to stick to trails and avoid walking directly through tall grass.
- Use insect repellents. Apply insect repellent with 20 percent or higher concentration of DEET (diethyltoluamide) to the skin. Apply to children and avoid the hands, mouth, and eyes. Follow all instructions. Apply products with permethrin to clothing or buy pretreated clothing.
- Tick-proof your yard. Cut down tall grass, weeds, or bushes where ticks live.
- Check for ticks. After potential exposure to ticks, check yourself, your children, and your pets. Remember that young deer ticks are very tiny, so check thoroughly.
- Shower. Ticks sometimes remain on the skin before attaching themselves. Showering when you get home can help remove ticks that are not fully attached. Use a washcloth to help remove any ticks.
- Remove ticks as soon as possible. To remove a tick, use a pair of tweezers to gently grab the tick near the head or mouth. Do not squeeze or crush the tick. Pull it out steadily with even pressure to remove the entire tick. Sanitize the bite area with antiseptic, and wash your hands. You may want to seal the tick in a container, and place it in the freezer. If you do have symptoms that worsen over time, your doctor may want to see the tick.
If you have had Lyme disease before, you are not immune to getting it again. Follow the recommendations above to reduce your risk of getting Lyme disease a second time.
Diagnosis and Treatment of Lyme Disease
Diagnosis for Lyme disease can be difficult. The symptoms of Lyme disease are similar to symptoms of other diseases. Ticks that carry Lyme disease may also carry other diseases. Typically, the bull’s eye rash is a key indicator of Lyme disease.
Whether or not you have the rash, your doctor may ask about your medical history and if you have spent time outdoors in areas where Lyme disease is common.
There are specific lab tests that can be helpful in determining whether or not a person has Lyme disease. These tests identify antibodies to the bacteria that causes Lyme disease and can confirm a diagnosis. Tests include:
- Enzyme-linked immunosorbent assay (ELISA) test. This test is commonly used to detect Lyme disease because it detects antibodies to Borrelia burgdorferi. The ELISA test may not test positive in the early stages of Lyme disease, because the body has not yet built up the antibodies. This test has also been known to provide false positives, so it is used in conjunction with other tests/observations.
- Western blot test. After receiving a positive result for the ELISA test, the Western blot test is done to confirm a diagnosis. It tests for several proteins of Borrelia burgdorferi.
It can take the body a few weeks to develop antibodies to the disease. Therefore, these tests are most reliable a few weeks after the infection.
Once Lyme disease has been confirmed, antibiotics are used for treatment. The sooner that treatment starts, the faster the recovery will be.
Antibiotic treatment options include:
- Oral antibiotics are used to treat early-stage Lyme disease. Doctors usually prescribe a 14- to 21- day course of antibiotics. Adults and children over 8 typically take doxycycline. Younger children and woman who are pregnant or breast-feeding take amoxicillin or cefuroxime.
- Intravenous antibiotics may be used as treatment if Lyme disease has affected the central nervous system. A course of intravenous antibiotics may be used for 14 to 28 days.
Some medical practices may recommend bismacine, an injectable compound, to treat Lyme disease. Bismacine, also known as chromacine, is not approved by the Food and Drug Administration in the injectable form. It contains high levels of the metal bismuth and can cause bismuth poisoning, which can lead to heart and kidney failure.
After treatment, some people may still experience mild symptoms, such as muscle aches and fatigue. This is known as post-treatment Lyme disease syndrome. The cause of these lingering symptoms is still unknown.
For individuals who have been diagnosed with Lyme disease or those seeking ongoing treatment for post-treatment Lyme disease syndrome (PTLDS), a private duty nurse can help with antibiotic infusions. NurseRegistry has skilled nurses that can administer antibiotic intravenous therapies in the comfort of home. If you would like to learn more about how a skilled nurse can help with your Lyme disease recovery, call 650-462-1001 to speak with one of our Client Care Coordinators.
Resources
The Bay Area Lyme Foundation has a list of local Bay Area and online support groups.
The Children’s Lyme Disease Network (CLDN) has a list of Lyme disease organizations and other resources specifically for children.
The LymeLight Foundation has financial and educational resources.
LymeDisease.org has a list of international resources, along with other educational information.
Lyme Disease Association, Inc. has a valuable list educational and patient resources.
The International Lyme Disease and Associated Diseases Society has an extensive collection of current articles and resources.
For more information on Lyme disease, visit:
The Centers for Disease Control and Prevention (CDC) on Lyme Disease
American Nurse Today on Lyme Disease Prevention and Treatment
NursingSchoolHub.com on Lyme Disease (an excellent resource for licensed nurses and nursing students)
Disclaimer: The information provided in this article is not intended to diagnose health problems or take the place of professional medical advice or care you receive from a health care provider. A Lyme diagnosis must be confirmed with a licensed medical professional. Always consult your health care provider about symptoms, health problems, medications, and treatments.