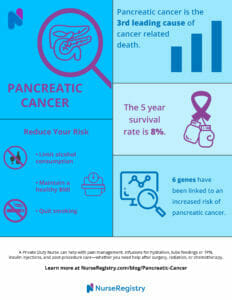
Pancreatic cancer is the third leading cause of cancer-related death in men and women. According to the American Cancer Society, it is predicted that 55,440 adults in the United States will be diagnosed with pancreatic cancer this year alone. As of now, the 5-year survival rate is 8 percent. Without a specific diagnostic test, pancreatic cancer can be difficult to diagnose.
The pancreas, an organ in the body that is located behind the stomach, helps with digestion and controls the metabolism of sugars throughout the body. It is comprised of exocrine and endocrine cells. The exocrine cells make up the exocrine glands and ducts. The endocrine cells make up smaller portions of the pancreas, such as islets. These islets create and release much-needed hormones—like glucagon and insulin—to help control blood sugar percentages.
Pancreatic cancer begins when the cells located in the pancreas grow at an enormously unusual rate. Much is known about pancreatic cancer, yet the illness in often diagnosed later in an individual’s life. The illness spreads very quickly to other parts of the body, and the prognosis can be difficult for medical professionals to determine.
Causes and Risk Factors
IN THIS ARTICLE
What is the risk for pancreatic cancer?
The exact cause of pancreatic cancer is unknown, but there are certain risk factors that can increase a person’s chances of developing the disease. Some of these risk factors include:
- Age: Pancreatic cancer is more common in people over the age of 60.
- Smoking: Cigarette smoking is a major risk factor for pancreatic cancer.
- Family history: About 10% of pancreatic cancers are hereditary, meaning they are caused by genetic mutations that are passed down through families.
- Obesity: Being overweight or obese can increase a person’s risk of developing pancreatic cancer.
- Chronic pancreatitis: Long-term inflammation of the pancreas can increase a person’s risk of developing pancreatic cancer.
Symptoms and Diagnosis of Pancreatic Cancer
Pancreatic cancer often does not cause symptoms in its early stages, which can make it difficult to diagnose. As the cancer grows, it can cause symptoms such as:
- Jaundice (yellowing of the skin and eyes)
- Abdominal pain or discomfort
- Unexplained weight loss
- Loss of appetite
- Nausea and vomiting
- Fatigue
If a doctor suspects pancreatic cancer, they may order imaging tests such as an ultrasound, MRI, or CT scan. A biopsy may also be performed to confirm the diagnosis.
Stages and Prognosis
Pancreatic cancer is staged based on how far it has spread in the body. The stages are:
- Stage 0: The cancer is only in the top layers of cells lining the pancreas.
- Stage I: The cancer is confined to the pancreas and has not spread to nearby lymph nodes or other organs.
- Stage II: The cancer has spread to nearby lymph nodes but has not spread to other organs.
- Stage III: The cancer has spread to nearby blood vessels and may have spread to nearby lymph nodes.
- Stage IV: The cancer has spread to other organs.
The prognosis for pancreatic cancer depends on the stage of the cancer and other factors such as the person’s age and overall health. Pancreatic cancer is often difficult to treat, but early detection and treatment can improve a person’s chances of survival.
Current Diagnosis
Pancreatic cancer is mainly diagnosed with the use of magnetic resonance imaging, computed tomography scans, endoscopic ultrasound, laparoscopy and biopsy. Yet, these test are not perfect and may miss small lesions and pre-cancers. There is not a specific tool used by medical professionals to detect the illness in the early stages. Early screening methods using a combination of tools are highly important for individuals with known pancreatic cancer in their family.
What about all the individuals who don’t have a family history of pancreatic cancer? Recently, a team discovered gene mutations linked to pancreatic cancer in people with and without a family history of the disease.
Over 3000 pancreatic cancer patients were seen for genetic testing at the Mayo Clinic over a sixteen year period. Twenty one cancer genes stood out to researchers; these were compared to genetic tests of nearly 125,000 patients without any sort of cancer.
They found six gene mutations related to an increased risk of pancreatic cancer. These mutations provide medical professionals and patients with a better estimate on the amount of cancer risk associated with each individual gene.
It’s important to note that researchers discovered the genetic mutations in individuals without a prior family history of pancreatic cancer. The genetic mutations were discovered in 5.5 percent of all individuals with pancreatic cancer, which includes those with and those without a family history of the disease. In pancreatic patients without a family history, 5.2 percent had the genetic mutations as well—a statistically significant number.
Fergus Couch, senior author for this study, says,
Genetic Factors in Pancreatic Cancer

Pancreatic cancer can be caused by various factors, including genetic mutations. In this section, we will discuss the genetic factors that contribute to the development of pancreatic cancer.
Hereditary Syndromes and Mutations
Several hereditary syndromes and mutations have been linked to pancreatic cancer. These include:
- Lynch syndrome: Also known as hereditary nonpolyposis colorectal cancer (HNPCC), this syndrome increases the risk of several types of cancer, including pancreatic cancer.
- BRCA1 and BRCA2 mutations: These mutations are commonly associated with breast and ovarian cancer, but they can also increase the risk of pancreatic cancer.
- CDKN2A mutations: This gene is responsible for producing a protein that helps regulate cell growth. Mutations in this gene can increase the risk of pancreatic cancer.
- PRSS1 mutations: This gene produces a protein called trypsinogen, which helps break down proteins in the pancreas. Mutations in this gene can lead to chronic pancreatitis and an increased risk of pancreatic cancer.
Genetic Testing and Screening
Genetic testing and screening can help identify individuals who are at a higher risk of developing pancreatic cancer due to genetic factors. Doctors may recommend genetic testing for individuals with a family history of pancreatic cancer or other cancers that are linked to hereditary syndromes.
Screening tests can also help detect pancreatic cancer early, when it is more treatable. The National Cancer Institute and the American Cancer Society recommend that individuals with a family history of pancreatic cancer or certain genetic syndromes undergo regular screening tests, such as endoscopic ultrasound or magnetic resonance imaging (MRI).
In conclusion, genetic factors can play a significant role in the development of pancreatic cancer. Individuals with a family history of pancreatic cancer or certain genetic mutations should consider genetic testing and regular screening to help detect the disease early.
Treatment Options and Management
Surgical and Non-Surgical Treatments
Pancreatic cancer treatment options depend on the stage of cancer, the patient’s overall health, and other factors. Surgery is often the first-line treatment for pancreatic cancer. A surgical oncologist may perform a Whipple procedure, which involves removing the head of the pancreas, the first part of the small intestine, the gallbladder, and sometimes part of the stomach. Other surgical options include distal pancreatectomy and total pancreatectomy.
First, creating a care plan is essential.
Non-surgical treatments for pancreatic cancer include chemotherapy and radiation therapy. Chemotherapy uses drugs to kill cancer cells, while radiation therapy uses high-energy radiation to destroy cancer cells. These treatments may be used alone or in combination with surgery.
Advancements in Therapies
Clinical trials are ongoing to develop new therapies for pancreatic cancer. The Precision Promise clinical trial, for example, is testing several new treatments for pancreatic cancer. Mayo Clinic is also conducting several clinical trials to test new therapies for pancreatic cancer.
Advancements in therapies have also led to the development of targeted therapies, which are drugs that target specific genes or proteins that are involved in cancer growth. These therapies may be more effective and have fewer side effects than traditional chemotherapy.
In summary, treatment options for pancreatic cancer include surgery, chemotherapy, and radiation therapy. Non-surgical treatments may be used alone or in combination with surgery. Clinical trials and targeted therapies are also being developed to improve treatment options for pancreatic cancer.
Lifestyle and Prevention
Pancreatic cancer is influenced by both genetic and lifestyle factors. While genetics plays a role in the development of pancreatic cancer, lifestyle factors such as smoking, obesity, and diet can also increase the risk of developing the disease. Therefore, making healthy lifestyle choices can help reduce the risk of developing pancreatic cancer.
Modifiable Risk Factors
Smoking
Smoking is one of the most significant risk factors for pancreatic cancer. According to the Pancreatic Cancer Action Network, smokers are two to three times more likely to develop pancreatic cancer than non-smokers. Therefore, quitting smoking is one of the most important things a person can do to reduce their risk of developing pancreatic cancer.
Obesity and Weight Loss
Obesity and weight gain are also risk factors for pancreatic cancer. Maintaining a healthy weight through regular exercise and a healthy diet can help reduce the risk of developing pancreatic cancer. In addition, losing weight if you are overweight or obese may also reduce the risk of developing pancreatic cancer.
Diet
A healthy diet is important for reducing the risk of developing pancreatic cancer. Eating a diet that is high in fruits, vegetables, and whole grains and low in red and processed meats may help reduce the risk of developing pancreatic cancer.
Age
Age is a risk factor for patients with pancreatic cancer, with most cases occurring in people over the age of 50. However, pancreatic cancer can occur at any age.
Diabetes and Pancreatitis
Diabetes and chronic pancreatitis are also risk factors for pancreatic cancer. Therefore, managing diabetes and treating pancreatitis may help reduce the risk of developing pancreatic cancer.
Inflammation
Inflammation is a risk factor for many types of cancer, including pancreatic cancer. Therefore, reducing inflammation through healthy lifestyle choices, such as regular exercise and a healthy diet, may help reduce the risk of developing pancreatic cancer.
Private Nursing Care for Pancreatic Cancer Patients
Do you have a loved one suffering from pancreatic cancer? NurseRegistry’s private nurses can help keep your loved one’s quality of life high from the comfort of their home. NurseRegistry’s private nurses have exceptional scheduling flexibility so you can receive a nurse whenever and wherever you need them.
Speaking of nurses, our nurses are only RNs or LVNs/LPNs, which means they are highly skilled, educated, and experienced in providing care.
Click below to learn more about NurseRegistry and how we could benefit your loved one suffering from pancreatic cancer today.
Frequently Asked Questions about Pancreatic Cancer
What genetic factors increase the risk of developing pancreatic cancer?
There are several genetic factors that can increase the risk of developing pancreatic cancer. Inherited gene mutations, such as the BRCA1 and BRCA2 genes, can significantly increase the risk of developing pancreatic cancer. Additionally, mutations in the CDKN2A, PALB2, and ATM genes have also been linked to an increased risk of pancreatic cancer.
Can having a family history of pancreatic cancer significantly raise one’s chances of diagnosis?
Yes, having a family history of pancreatic cancer can significantly raise one’s chances of diagnosis. Individuals with two or more first-degree relatives (parents, siblings, or children) who have been diagnosed with pancreatic cancer have a higher risk of developing the disease themselves.
Which gene mutations are most commonly associated with pancreatic cancer?
The most commonly associated gene mutations with pancreatic cancer are the BRCA1 and BRCA2 genes. These genes are also associated with an increased risk of breast and ovarian cancer.
How does the risk of pancreatic cancer differ between individuals with and without a family history?
Individuals with a family history of pancreatic cancer have a higher risk of developing the disease compared to those without a family history. The risk increases with the number of affected family members and the age at which they were diagnosed.
What are the recommended screening protocols for someone with a family history of pancreatic cancer?
For individuals with a family history of pancreatic cancer, the recommended screening protocol includes a yearly magnetic resonance imaging (MRI) or endoscopic ultrasound (EUS) starting at age 50, or 10 years prior to the youngest affected relative’s diagnosis.
What is the role of genetic testing in assessing pancreatic cancer risk?
Genetic testing can help identify individuals with an increased risk of developing pancreatic cancer. It can also help determine if family members are carriers of inherited gene mutations and may benefit from early screening and surveillance.
What is the average age of pancreatic cancer death?
The average age of pancreatic cancer death is around 72 years old.
What is the life expectancy with pancreatic cancer?
The life expectancy of pancreatic cancer varies depending on the stage at diagnosis. The overall five-year survival rate for pancreatic cancer is around 10%. However, for those diagnosed at an early stage, the five-year survival rate can be as high as 37%.
Gloria Peterson, researcher and senior author for the Mayo Clinic, believes genetic testing should be performed on all patients, rather than just the ones with a family history of pancreatic cancer, which is the current standard of care. In the future, genetic testing will allow for an easier and earlier diagnosis of pancreatic cancer than the methods currently used by medical professionals.
If you or a loved one has received a pancreatic cancer diagnosis, learn how a private duty nurse from NurseRegistry can help. Our full list of services is available on our private care page.
Resources
Find out more about the research study at Medical Press.
Mayoclinic.org offers many resources and information about pancreatic cancer.
American Cancer Society is another great resource for pancreatic cancer.
The Pancreatic Cancer Action Network provides useful information about pancreatic cancer.
Disclaimer: The information provided in this article is not intended to diagnose health problems or take the place of professional medical advice or care you receive from a health care provider. A pancreatic cancer diagnosis must be confirmed with a licensed medical professional. Always consult your health care provider about symptoms, health problems, medications, and treatment.
Written by Jesse Rio






